Background: 42-year-old patient presents to clinic with asymptomatic hypercalcemia. The calcium level is elevated at 12.4 mg/dL. PTH is normal. The 25 and 1,25 vitamin D levels are normal. The magnesium level is 2.8 mEq/L. The 24 hour urine calcium level is low. There is no evidence of cancer.
Please answer the following questions:
What is the diagnosis?
* primary hyperparathyroidism
* familial hypocalciuric hypercalcemia
* vitamin D-dependent rickets
* laboratory error
familial hypocalciuric hypercalcemia
Describe familial hypocalciuric hypercalcemia (FHH).
FHH is an autosomal dominant disorder caused by an inactivating mutation in the calcium-sensing receptor (CaSR), leading to increased calcium reabsorption from renal tubules and resulting in hypercalcemia and hypocalciuria.
How does the CaSR gene mutation affect calcium levels in patients with FHH?
The CaSR gene mutation increases calcium reabsorption from renal tubules, causing approximately 99% of filtered calcium to be reabsorbed, despite hypercalcemia being present in the body.
Mutations in the CaSR gene disrupt the normal feedback mechanism that regulates calcium homeostasis. This leads to an inability to sense elevated calcium levels, resulting in excessive reabsorption in the kidneys.
Define the role of the calcium-sensing receptor in the parathyroid glands for patients with FHH.
In patients with FHH, there is a loss-of-function mutation in the calcium-sensing receptors of the parathyroid glands, which increases the set point of the glands and reduces their sensitivity to high serum calcium levels.
What laboratory abnormalities are typically seen in patients with FHH?
Patients with FHH typically present with elevated calcium, hypocalciuria, inappropriately normal or elevated parathyroid hormone (PTH) levels, and elevated magnesium levels.
How does FHH differ from primary hyperparathyroidism in terms of PTH levels?
Unlike primary hyperparathyroidism, most patients with FHH do not have significant elevations in serum PTH levels.
FHH is a genetic condition affecting calcium sensing, leading to normal or low PTH levels despite elevated calcium. In contrast, primary hyperparathyroidism typically is a result of high PTH levels because of overactivity of the parathyroid glands. This distinction is crucial for accurate diagnosis and management.
What is the typical treatment approach for patients diagnosed with FHH?
Most patients with FHH do not require treatment, as they are typically asymptomatic and do not need a parathyroidectomy.
Familial hypocalciuric hypercalcemia (FHH) is often benign, with numerous individuals remaining asymptomatic throughout their lives. Monitoring calcium levels and renal function is usually sufficient, as invasive treatments like parathyroidectomy are unnecessary and could lead to complications in these patients.
Explain the significance of hypocalciuria in FHH
Hypocalciuria in FHH indicates low urinary calcium excretion despite high serum calcium levels, which is a key characteristic of the disorder.
Hypocalciuria is crucial in differentiating Familial Hypocalciuric Hypercalcemia (FHH) from other conditions like primary hyperparathyroidism. It reflects the kidneys’ impaired ability to excrete calcium, leading to elevated serum calcium levels. This unique renal handling of calcium helps guide diagnosis and management strategies.
Describe the genetic mechanisms that cause familial hypocalciuric hypercalcemia (FHH).
FHH is caused by inactivating mutations in the calcium-sensing receptor, the G-protein subunit α11, or adaptor-related protein complex 2, sigma 1 subunit.
Familial hypocalciuric hypercalcemia (FHH) results from disrupted calcium homeostasis due to mutations affecting the calcium-sensing receptor, which normally regulates parathyroid hormone secretion. This leads to increased calcium reabsorption in the kidneys and altered calcium levels in the blood, causing hypercalcemia.
What should be included in the initial workup of hypercalcemia to aid in diagnosis?
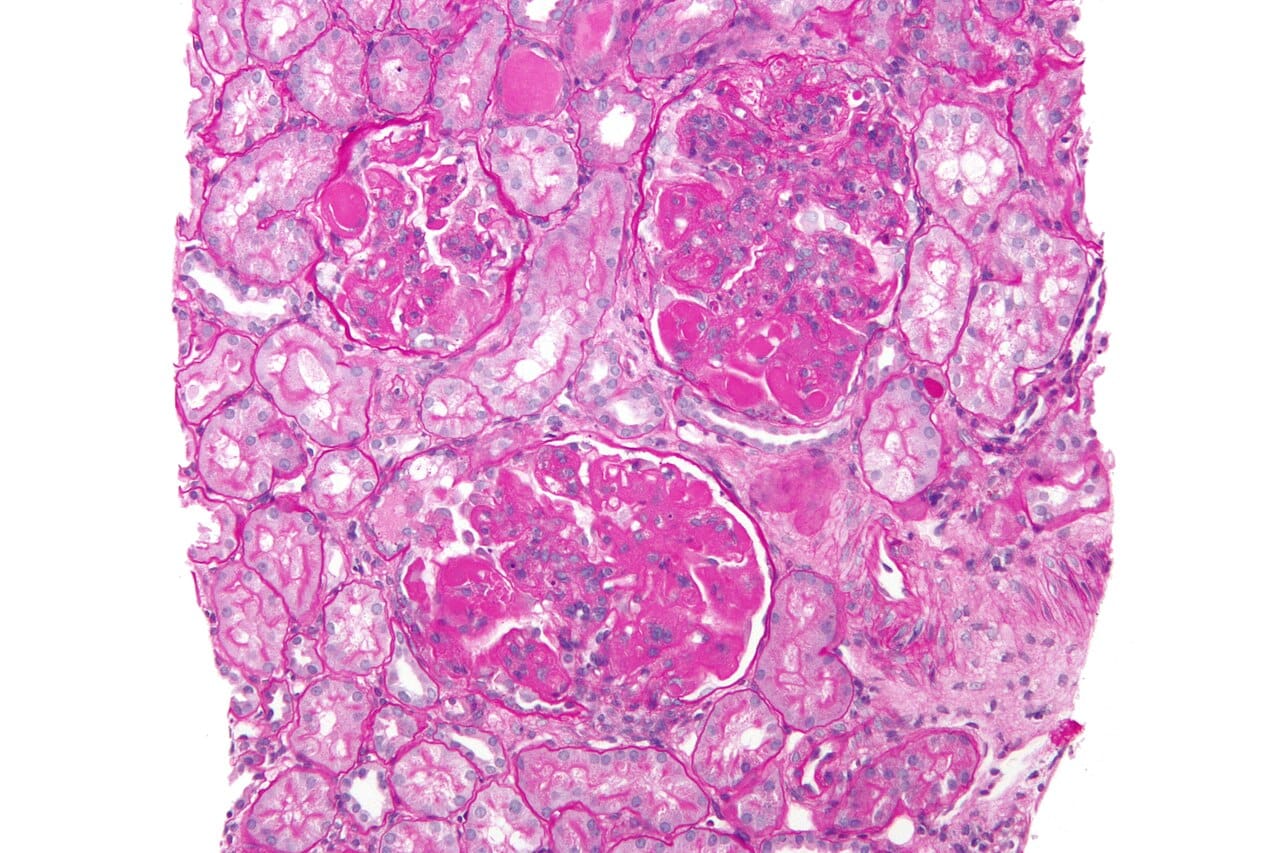
The initial workup of hypercalcemia should include 24-hour urine calcium and/or urinary calcium to creatinine measurements.
Measuring 24-hour urine calcium helps differentiate between primary hyperparathyroidism and other causes of hypercalcemia. Elevated urine calcium suggests primary hyperparathyroidism. Increased calcium in the urine is also seen in malignancy, which this patient did not have. Creatinine levels assess kidney function, crucial for interpreting calcium excretion.
What treatment has been used for symptomatic causes of familial hypocalciuric hypercalcemia (FHH)?
The calcimimetic cinacalcet has been used to treat hypercalcemia in certain symptomatic cases of FHH.
Cinacalcet acts by increasing the sensitivity of calcium-sensing receptors, which helps lower parathyroid hormone levels and subsequently reduces calcium levels in the blood. This mechanism is beneficial in managing hypercalcemia associated with FHH, where traditional treatments may be less effective.
Why is this presentation not consistent with vitamin D dependent rickets or laboratory error?
The vitamin D level is normal. The presentation is consistent with FHH, suggesting the laboratory studies are correct.
Discussion:
Related Posts:
Edema Treatment – On Steroids For Minimal Change Disease – Has High Blood Pressure – Test by Michael Aaronson MD, Lincoln Nephrology and Hypertension
Patient With An Adrenal Adenoma And Hypertension – What is the Cause? by Michael Aaronson, Lincoln Nephrology and Hypertension