Acute Interstitial Nephritis Case:
Background: An older woman was started on therapy for temporal arteritis 4 months ago. Medications include prednisone, omeprazole, empagliflozin, and vitamin D. The patient’s temporal arteritis improved, but she did not feel well. The primary provider worked up the condition, noting an increase in the serum creatinine, and a urine which showed leukocytes. The patient was treated for a presumed urinary tract infection. Results of the urine culture were negative. She is diagnosed with acute interstitial nephritis.
The creatinine was 2.1 mg/dL (baseline 1.3). The CBC revealed the presence of eosinophils. The patient does not have a rash or a fever.
Please answer the following questions:
Which medication most likely caused the acute interstitial nephritis?
* empaglifozen
* vitamin D
* omeprazole
* prednisone
omeprazole
Describe acute interstitial nephritis (AIN).
AIN is a kidney condition typically caused by a hypersensitivity reaction to medications, especially antibiotics, proton pump inhibitors, or NSAIDs.
Acute interstitial nephritis (AIN) involves inflammation of the kidney’s interstitium, often triggered by drug reactions. This condition can lead to impaired kidney function and may present with symptoms like fever, rash, or eosinophilia. Early recognition and discontinuation of the offending agent are crucial for recovery.
Our patient had AIN subacutely caused by the proton pump inhibitor omeprazole. The most likely reason the patient did not present with fever or rash is because she was on prednisone for her temporal arteritis.
How does the clinical presentation of AIN vary?
The clinical presentation of AIN varies depending on the precipitating medication, but classic symptoms include fever, rash, and eosinophilia, often with elevated serum creatinine.
Acute interstitial nephritis (AIN) can manifest differently based on the specific drug involved, as each medication may trigger unique immune responses. The presence of fever and rash indicates systemic involvement, while eosinophilia suggests an allergic reaction, highlighting the importance of early recognition for effective management.
Define the classic triad of symptoms associated with AIN.
The classic triad of symptoms for AIN includes fever, rash, and eosinophilia, although triad is only present in about 10% of cases.
AIN usually presents with a diverse range of symptoms, making diagnosis challenging. The classic triad highlights key indicators that can guide clinicians, but its low occurrence emphasizes the need for comprehensive evaluation of patient history and laboratory findings to ensure accurate diagnosis and management.
What is the significance of medication exposure in diagnosing AIN?
Exposure to a culprit medication is often the most compelling sign of AIN, requiring a high index of suspicion from physicians.
Exposure to a therapy in the past can cause a sudden onset of symptoms. Certain medicines, like proton pump inhibitors, can lead to a more gradual development of symptoms.
How long after drug exposure does AIN typically occur?
AIN generally occurs after 7 to 10 days of drug exposure, but this timing can vary.
Acute interstitial nephritis (AIN) is an immune-mediated response often triggered by medications. The 7 to 10-day window reflects the time needed for the immune system to recognize and react to the drug, leading to inflammation. Individual variability in immune response can influence this timing
What might previous exposure to a drug indicate in AIN?
Previous exposure to a drug may lead to a more sudden onset of AIN symptoms.
Previous drug exposure can sensitize the immune system, potentially triggering a quicker inflammatory response. This heightened reactivity may cause a rapid manifestation of acute interstitial nephritis (AIN) symptoms, emphasizing the importance of patient history in diagnosing renal conditions.
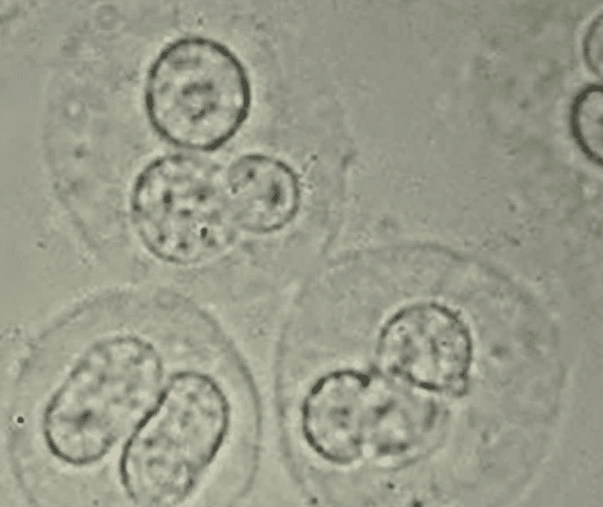
What are common findings seen in the urinalysis for AIN?
The urinalysis in AIN may reveal leukocytes, leukocyte casts with negative urine cultures (sterile pyuria), and/or erythrocytes.
Acute interstitial nephritis (AIN) often presents with inflammation, leading to the presence of leukocytes and casts in urine. The sterile pyuria indicates an immune response rather than a bacterial infection, while erythrocytes may suggest glomerular involvement or injury. These findings help differentiate AIN from other renal conditions.
What is the mainstay treatment for AIN?
The mainstay treatment for AIN is the discontinuation of the offending agent.
Discontinuing the offending agent is crucial because it addresses the root cause of acute interstitial nephritis (AIN). This condition often arises from drug reactions, and removing the trigger can halt further kidney damage, allowing for recovery. Supportive care, including the use of steroids, may also be necessary to manage symptoms and restore kidney function.
How does the presentation of AIN relate to proton pump inhibitors?
In this case, the patient has elevated serum creatinine levels and sterile pyuria following exposure to the proton pump inhibitor omeprazole, making AIN the most likely diagnosis.
Acute interstitial nephritis (AIN) can occur as an adverse reaction to medications, including proton pump inhibitors (PPIs). The combination of elevated serum creatinine and sterile pyuria suggests an inflammatory process in the kidneys, often triggered by drug exposure, highlighting the need for careful monitoring in patients on PPIs.
Explain the potential consequences of untreated drug-induced AIN.
If left untreated, drug-induced AIN can lead to permanent renal insufficiency or even end-stage kidney disease (ESKD).
Untreated drug-induced acute interstitial nephritis (AIN) can result in significant kidney damage, as the inflammation may progress and impair renal function. This can disrupt electrolyte balance, waste elimination, and overall homeostasis, potentially necessitating dialysis or transplantation in severe cases. Early intervention is crucial.
What is the definition of AIN in terms of serum creatinine levels?
AIN is defined as an increase of 0.5 mg/dL or 50% in serum creatinine over a 24- to 72-hour period, starting 24 to 48 hours after exposure to a potential triggering medication.
Describe medications associated with acute interstitial nephritis.
Medications associated with acute interstitial nephritis include proton pump inhibitors (e.g., omeprazole, lansoprazole), H2 blockers (e.g., cimetidine), allopurinol, penicillins, cephalosporins, rifampin, ciprofloxacin, trimethoprim-sulfa, NSAIDs, diuretics, and immune checkpoint inhibitors (e.g., ipilimumab, nivolumab).
What is the prognosis for acute interstitial nephritis with early recognition and treatment?
With early recognition and proper treatment, acute interstitial nephritis and its associated kidney failure are generally reversible.
Do glucocorticoids play a role in the treatment of acute interstitial nephritis?
Glucocorticoid therapy can be considered in selected patients with biopsy-proven acute interstitial nephritis, in addition to the withdrawal of the offending agent.
Glucocorticoids help reduce inflammation in acute interstitial nephritis, particularly when the condition is severe or persistent despite removing the causative agent. Their immunosuppressive properties can aid recovery by modulating the immune response, potentially improving kidney function in affected individuals.
NSAID-induced acute interstitial nephritis may not respond to glucocorticoid therapy, unlike other forms of AIN. NSAID-induced acute interstitial nephritis often involves a unique inflammatory response that may not be as effectively modulated by glucocorticoids. This resistance can stem from the specific mechanisms of injury caused by NSAIDs, which may require alternative therapeutic approaches for resolution.
Discussion:
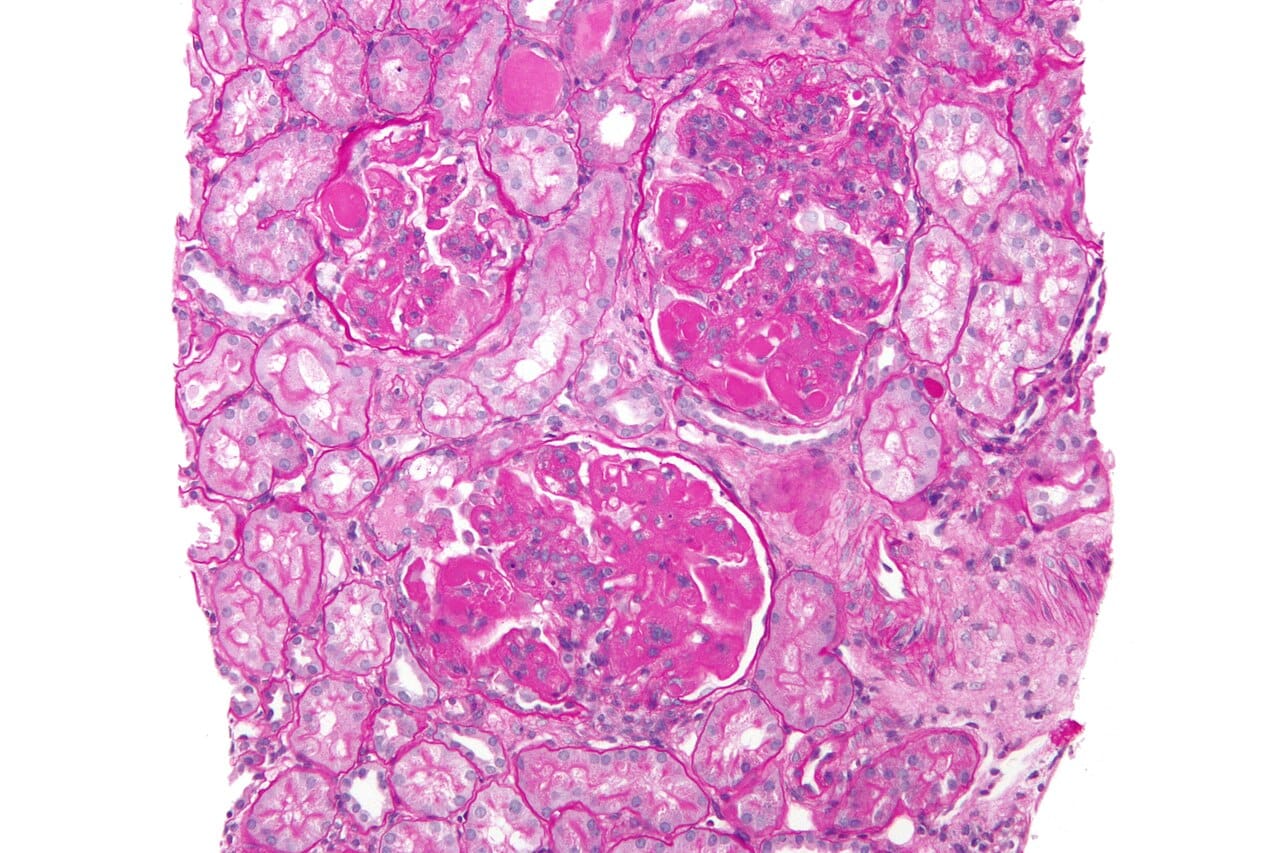
Acute Interstitial Nephritis (AIN)
Diagnosis and Causes
AIN is often caused by a hypersensitivity reaction to medications like antibiotics, proton pump inhibitors, or NSAIDs.
- The clinical presentation varies but may include fever, rash, eosinophilia, and elevated serum creatinine.
- AIN is mainly triggered by drug exposure, with proton pump inhibitors linked to a more subacute course.
Signs and Symptoms
Urinalysis may reveal leukocytes, leukocyte casts, sterile pyuria, and/or erythrocytes.
Treatment and Prognosis
The mainstay of treatment is discontinuation of the offending medication.
- Early recognition and withdrawal of the causative drug can lead to reversibility of AIN and renal failure.
- Glucocorticoid therapy may be considered in selected patients with biopsy-proven AIN, except for NSAID-induced cases.
Drug Associations
Medications linked to AIN include proton pump inhibitors, H2 blockers, penicillins, cephalosporins, NSAIDs, diuretics, and immune checkpoint inhibitors.
Statistics and Complications
Drug-induced AIN accounts for 70-75% of cases in developed countries and is responsible for approximately 20% of renal biopsies for unexplained AKI.
- AIN is defined by a significant increase in serum creatinine after exposure to a potential triggering medication.
- It can lead to acute decline in renal function, potentially progressing to permanent kidney insufficiency or end-stage kidney disease.
Inspiration: Allergic and Drug-Induced Interstitial Nephritis, National Library of Medicine
Related Posts:
Urinary Frequency, Dysuria, Urgency Post Starting SGLT2 Inhibitor – Provider Quiz by Michael Aaronson MD