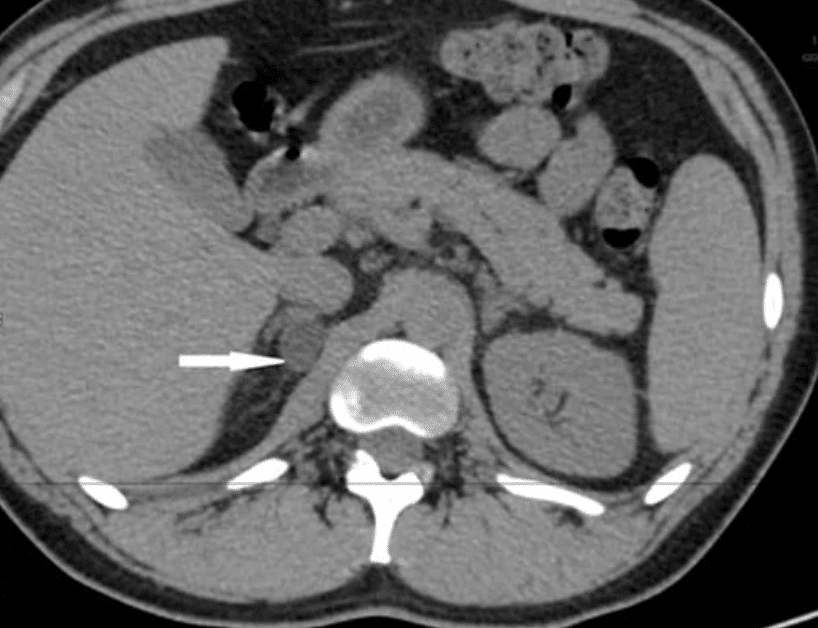
Background: A 28-year-old male presents to the nephrologist’s clinic for hard to control hypertension. Physical examination is unremarkable. The patient has a blood pressure of 182/91 on multiple medications. Labs reveal hypokalemia and metabolic alkalosis. Renin levels are suppressed. Aldosterone levels are elevated. The plasma aldosterone activity to plasma renin activity is greater than 20. CT shows a small, right adrenal adenoma.

Please answer the following questions:
What diagnosis should be high up on your differential in this patient with a functional adrenal adenoma?
* Cushing’s syndrome
* Primary Aldosteronism
* Sarcoidosis
* Addison’s disease
* Milk-alkali syndrome
Primary Aldosteronism
Describe adrenal adenomas and their characteristics.
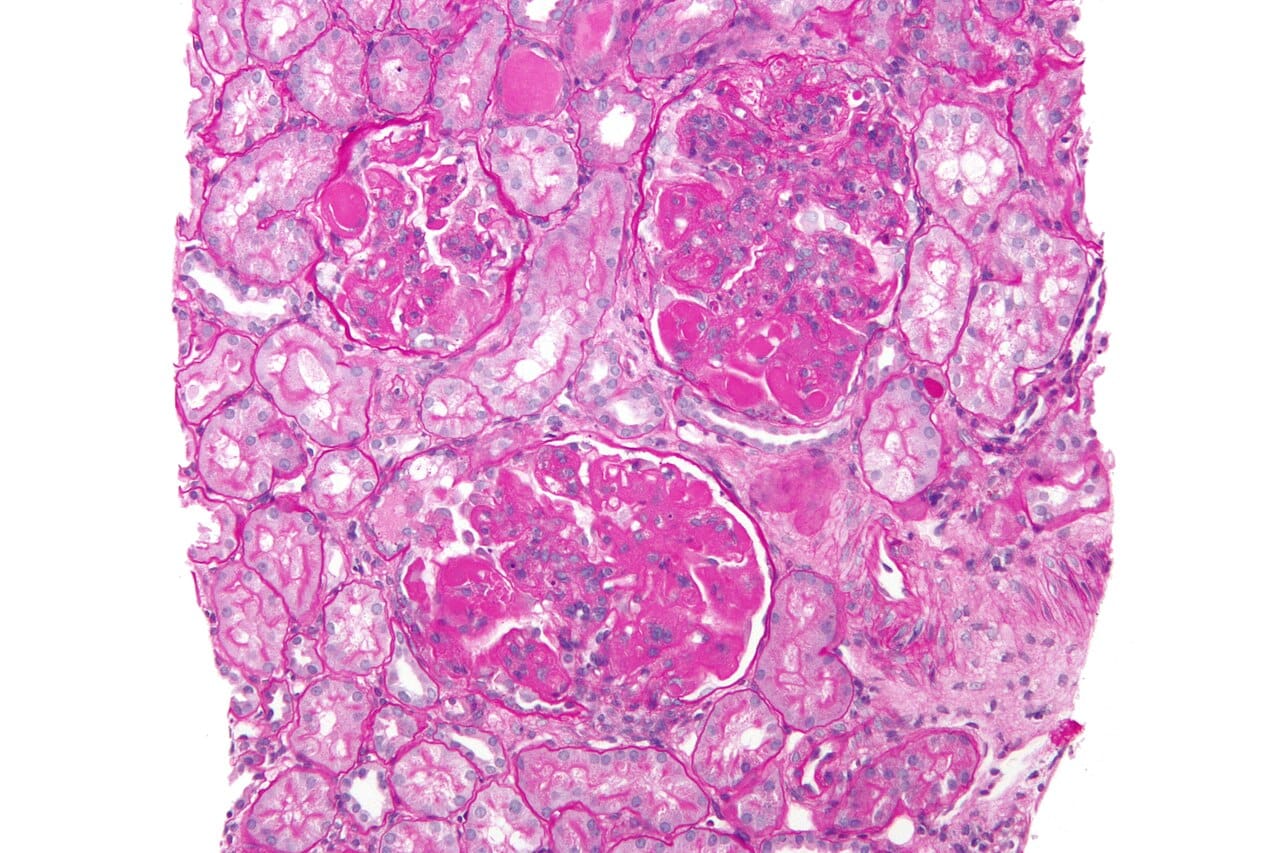
Adrenal adenomas are benign neoplasms that originate from the adrenal cortex. They can be categorized as non-secreting or functional, with functional adenomas often presenting symptoms related to hormonal activity.
Adrenal adenomas are significant because of their potential impact on hormonal balance. Functional adenomas can lead to conditions like Cushing’s syndrome or primary hyperaldosteronism, affecting metabolism and blood pressure. Their benign nature contrasts with malignant adrenal tumors, making diagnosis and management crucial for patient health.
How are adrenal adenomas evaluated?
The evaluation of an adrenal adenoma requires a comprehensive approach involving imaging and hormonal workup.
Define primary aldosteronism and its key features.
Primary aldosteronism is characterized by increased aldosterone secretion from the adrenal glands, suppressed plasma renin activity, hypertension, and hypokalemia.
Primary aldosteronism, often linked to adrenal tumors or hyperplasia, leads to excessive sodium retention and potassium loss, resulting in hypertension and low potassium levels. This condition can cause cardiovascular complications if untreated, highlighting the importance of early diagnosis and management.
What are the two major subtypes of primary hyperaldosteronism?
The two major subtypes of primary hyperaldosteronism are unilateral aldosterone-producing adenoma (APA) and idiopathic hyperaldosteronism (IHA) or bilateral adrenal hyperplasia
Primary hyperaldosteronism is characterized by excessive aldosterone production, leading to hypertension and electrolyte imbalances. Unilateral aldosterone-producing adenoma typically involves a single tumor, while idiopathic hyperaldosteronism often results from diffuse adrenal hyperplasia, affecting both adrenal glands. Understanding these subtypes aids in targeted treatment strategies.
How does aldosterone affect renal function?
Aldosterone induces renal distal tubular reabsorption of sodium, enhancing the secretion of potassium and hydrogen ions, which can lead to hypernatremia, hypokalemia, and alkalosis.
Aldosterone plays a crucial role in maintaining electrolyte balance and blood pressure. By promoting sodium reabsorption, it helps regulate fluid volume, while the increased potassium and hydrogen ion secretion can significantly impact acid-base balance, potentially leading to various metabolic disturbances.
Describe the symptoms associated with severe hypokalemia.
Patients with severe hypokalemia can experience fatigue, muscle weakness, cramping, headaches, palpitations, polydipsia, and polyuria because of nephrogenic diabetes insipidus.
What is the typical management for small, hormonally inactive adrenal adenomas?
Small adenomas that are hormonally inactive usually require routine follow-up examinations without immediate intervention.
Small, hormonally inactive adrenal adenomas rarely cause symptoms or hormonal imbalances, making invasive treatments unnecessary. Regular monitoring helps ensure any changes in size or function are detected early, allowing for timely intervention if needed, while minimizing risks associated with surgery.
Explain the relationship between hypokalemia and metabolic alkalosis in primary aldosteronism.
Hypokalemia in primary aldosteronism can lead to metabolic alkalosis, as the increased aldosterone causes enhanced secretion of potassium and hydrogen ions.
In primary aldosteronism, excess aldosterone promotes sodium retention and potassium excretion. Losing hydrogen ions alongside potassium contributes to a rise in blood pH, resulting in metabolic alkalosis. This interplay highlights the intricate balance of electrolytes and acid-base status in endocrine disorders.
How can hormonally active adrenal adenomas present clinically?
Adenomas that exhibit significant hormonal activity can present with characteristic symptoms of Cushing’s syndrome, primary hyperaldosteronism, or pheochromocytoma.
Regarding primary hyperaldosteronism: describe the effects of pronounced alkalosis on calcium levels in the body.
Pronounced alkalosis enhances calcium binding to albumin, leading to relative hypocalcemia, which can cause symptoms such as numbness, tingling in the extremities and perioral area, muscle cramps, carpopedal spasm, and in extreme cases, laryngeal spasm and convulsions.
Alkalosis alters the ionization of calcium in the blood, increasing its binding to proteins like albumin. This shift results in lower free calcium levels, which are crucial for various physiological functions, including nerve transmission and muscle contraction. The symptoms reflect the body’s response to decreased ionized calcium.
What are the typical renin levels in patients with primary hyperaldosteronism?
In patients with primary hyperaldosteronism, renin levels are typically suppressed to less than 1 ng/mL/h and do not exceed 2 ng/mL/h with diuretics and upright posture.
In primary hyperaldosteronism, the adrenal glands produce excess aldosterone, leading to sodium retention and potassium excretion. This results in low renin levels because of negative feedback, as the body senses high blood volume and pressure.
How can the sensitivity of a screening test for primary hyperaldosteronism be improved?
The sensitivity of a screening test for primary hyperaldosteronism can be improved by calculating the ratio of plasma aldosterone (PA) activity to plasma renin activity (PRA). A PA-to-PRA ratio greater than 20 (with a PA greater than 15 ng/dL) represents a sensitivity of 100% and a specificity of 80%
Improving sensitivity in screening tests often involves refining the criteria used for diagnosis. The PA-to-PRA ratio effectively highlights the hormonal imbalance characteristic of primary hyperaldosteronism, allowing for more accurate identification of affected individuals, thus enhancing early detection and management.
Describe the symptoms associated with Cushing’s syndrome.
Cushing’s syndrome can cause symptoms such as moon facies, facial plethora, supraclavicular fat pads, buffalo hump, truncal obesity, purple striae, proximal muscle weakness, easy bruising, weight gain, hirsutism, and growth retardation in children.
Cushing’s syndrome results from excess cortisol, leading to distinctive physical changes and metabolic issues. The symptoms reflect alterations in fat distribution, skin integrity, and muscle strength.
What causes Cushing’s syndrome?
Cushing’s syndrome is caused by prolonged exposure to elevated levels of either endogenous or exogenous glucocorticoids.
Cushing’s syndrome results from an imbalance in cortisol levels, which can stem from various sources. Endogenous causes include adrenal tumors or pituitary adenomas, while exogenous sources often involve long-term corticosteroid medication.
Describe the common causes of Cushing’s syndrome.
The most common cause of Cushing’s syndrome is the use of exogenous glucocorticoids.
How can exogenous steroids affect the hypothalamic-pituitary-adrenal (HPA) axis?
Exogenous steroids may cause suppression of the HPA axis that can last for as long as a year after steroid administration has ended.
Exogenous steroids can disrupt the natural feedback mechanisms of the HPA axis, leading to decreased endogenous steroid production. This suppression can cause adrenal insufficiency, affecting stress response and overall hormonal balance, which may take time to recover even after steroid use has ceased.
Define Addison’s disease
Addison’s disease involves adrenocortical insufficiency because of the destruction or dysfunction of the entire adrenal cortex, affecting both glucocorticoid and mineralocorticoid function.
What is sarcoidosis?
Sarcoidosis is a multisystem inflammatory disease of unknown etiology that predominantly affects the lungs and intrathoracic lymph nodes.
Sarcoidosis often presents with granulomas, which are clusters of immune cells that form in response to inflammation. While the exact cause remains elusive, genetic, environmental, and infectious factors may play a role.
Define milk-alkali syndrome.
Milk-alkali syndrome is caused by the ingestion of large amounts of calcium and absorbable alkali, leading to hypercalcemia.
Discussion:
Enjoyed Learning about adrenal adenoma? Learn more by reading our Related Posts:
Nephrology Test: Hypercalcemia In An Asymptomatic Patient – by Michael Aaronson