Background:
64-year-old with an upper respiratory tract infection is evaluated in the clinic. He has a history of high blood pressure. His intake has been poor the last few days. Current medications include amlodipine, irbesartan, and hydrochlorothiazide. He has no focal neurologic signs. The blood pressure is 111/67. There is no swelling. He appears euvolemic, and the serum sodium is noted to be 121. The bun is 8, potassium 3.1. Urine osmolality and other appropriate studies are pending.
Please answer the following questions:
What is the most likely diagnosis?
Euvolemic (isovolemic), chronic, hypotonic hyponatremia.
Patient follow up: the serum osmolality (osm) came back at 242. The urine osm was 480.
Assume that this is the correct diagnosis as you work through the following questions and review the discussion below.
What is the next step?
* Admit for iv fluid (either hypertonic saline or normal saline based on lab results)
* Stop the hydrochlorothiazide and fluid restrict. Admit.
* Order tolvaptan
* Give him some salt tablets
Stop the hydrochlorothiazide and fluid restrict. Admit.
This is an appropriate starting management strategy.
Chronic hyponatremia is defined as a drop in serum sodium in less than 48 hours.
A
True
B
False
False
This is acute hyponatremia.
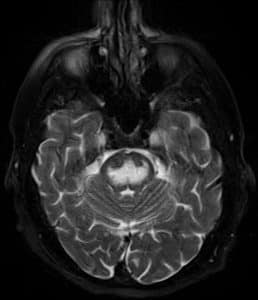
Rapidly increasing serum sodium levels in patients with chronic hyponatremia can lead to osmotic demyelination syndrome (ODS).
A
True
B
False
True
See the discussion below for a picture, brain MRI, of what osmotic demyelination looks like.
Hypertonic saline, 3%, is an appropriate management strategy for symptomatic and acute isovolemic hypotonic hyponatremia?
A
True
B
False
True
Is administering 0.9% saline an effective treatment for isovolemic hypotonic hyponatremia in the patient described above?
A
True
B
False
False
Providing intravenous normal saline can treat hypovolemic hypotonic hyponatremia but does not benefit a patient with isovolemic hypotonic hyponatremia.
Discussion:
Related Posts: