Acute Kidney Injury and Vancomycin Nephrotoxicity
Overview of Acute Kidney Injury (AKI)
Acute kidney injury (AKI) is a sudden decrease in kidney function, which can be caused by various factors. In hospital settings, the most common cause of AKI is acute tubular necrosis (ATN), characterized by damage to renal tubular epithelial cells. This damage is often because of ischemia or exposure to nephrotoxins.
Causes of Acute Tubular Necrosis (ATN)
ATN can be identified through careful evaluation of:
* Hemodynamics, volume status, and medications
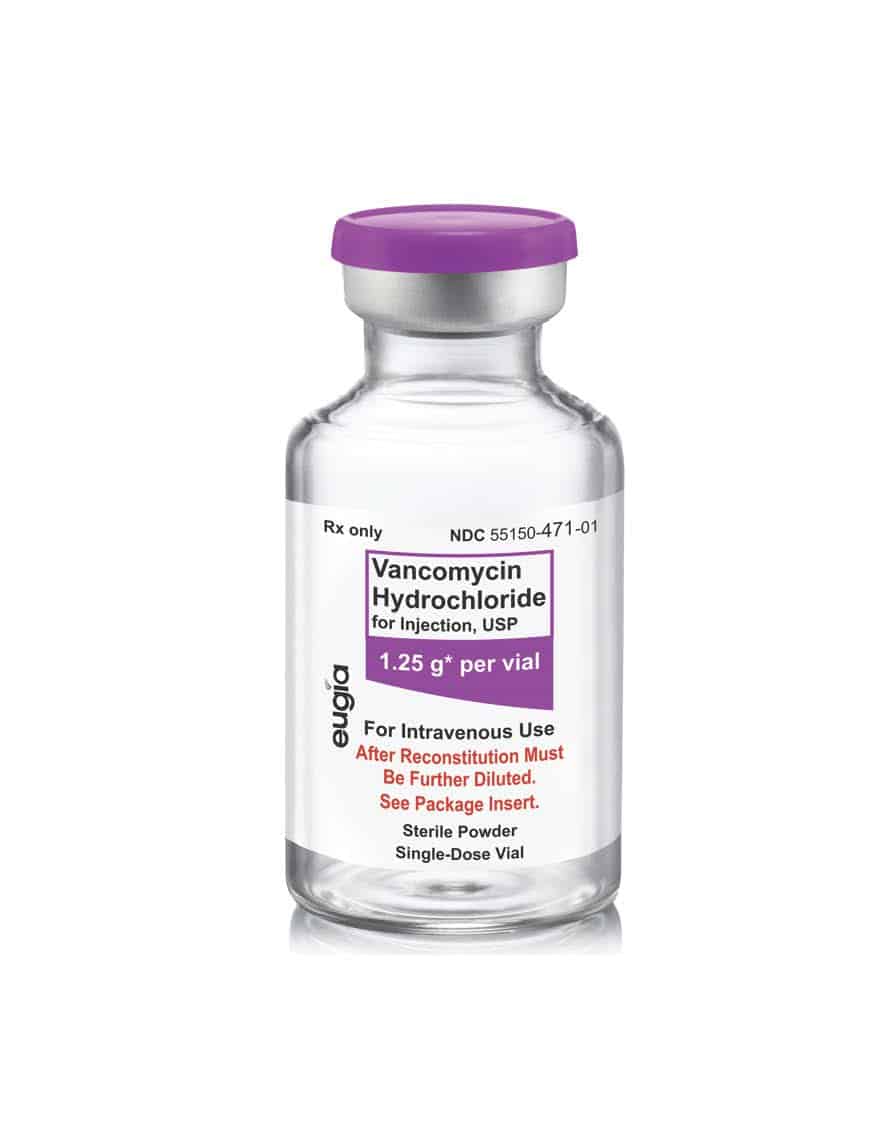
Vancomycin can cause of AKI in patients, with most reported cases linked to acute interstitial nephritis (AIN). However, ATN has also been documented in patients receiving vancomycin.
Indicators of ATN
Diagnosis of ATN is supported by:
* Rapid rise in serum creatinine levels
* Fractional excretion of sodium greater than 2%
* Urine microscopy demonstrating numerous renal tubular epithelial cells and granular casts
Risk Factors for Vancomycin Nephrotoxicity
* Several risk factors increase the likelihood of vancomycin nephrotoxicity, including:
* Chronic kidney disease
* Prolonged therapy with vancomycin
* Doses of vancomycin ≥ 4 grams per day
* Trough concentrations of vancomycin > 15 mg/L
Concurrent use of loop diuretics or other nephrotoxins, such as concomitant use of piperacillin-tazobactam
* Early recognition and prompt discontinuation of vancomycin is crucial for kidney recovery.
* Concurrent Nephrotoxin Exposure in vancomycin nephrotoxicity
Patients receiving vancomycin, particularly in ICU settings, may also be exposed to other nephrotoxic agents, which can further compromise kidney function. These include:
* Proton pump inhibitors, other antibiotics such as piperacillin-tazobactam, Acyclovir, calcineurin inhibitors, chemotherapy agents, intravenous contrast, vasopressors, loop diuretics, Renin-angiotensin system blockers
Acute Interstitial Nephritis (AIN)
AIN can be caused by certain antibiotics, such as piperacillin-tazobactam, and proton pump inhibitors like omeprazole.
AIN may also be associated with:
* Drugs, infections, autoimmune diseases, and malignancy
Only 10% to 30% of patients with AIN exhibit the classic triad of symptoms, which includes fever, rash, and eosinophilia. Urine chemistries may show variable fractional excretion of sodium, while urinalysis may reveal:
* Hematuria, pyuria, leukocyte casts, and possibly eosinophiluria (not a reliable diagnostic marker). Nephrologists no longer suggest ordering this study to evaluate for acute interstitial nephritis.
Drug-induced AIN typically presents with a gradual increase in serum creatinine levels 7 to 10 days post-exposure, but can occur within 1 day if there has been prior exposure. It may also manifest months after exposure, particularly with NSAIDs and proton pump inhibitors. Here, the patient’s urinalysis findings do not support AIN.
Contrast-Induced Nephropathy (CIN)
Contrast-induced nephropathy (CIN) leads to ATN, with serum creatinine levels rising within 48 hours of contrast exposure. However, the patient in question did not receive any contrast, ruling out CIN as a cause of AKI.